How a Cardiac Perfusion Technology Keeps You Alive? [2025]

Cardiac Perfusion Technology Explained

Life Support Beyond the Body Cardiac Perfusion Technology
Imagine your heart stopped beating during surgery.
Your lungs stop breathing.
But you’re still alive.
That’s the miracle of the heart-lung machine.
Also known as a cardiopulmonary bypass (CPB) machine, this device temporarily takes over the heart’s pumping and the lungs’ oxygen exchange. It gives your heart a chance to rest or undergo surgery without depriving your body of oxygen-rich blood.
Used in millions of surgeries worldwide, it’s one of medicine’s most life-saving inventions.
In the following sections, we’ll explore how it works, why it’s used, its impact on recovery, and what it means for your long-term health.
What Is Cardiac Perfusion Technology and How Does It Work?
A cardiac perfusion technology is a medical device used during open-heart surgeries. It keeps you alive when your heart is stopped.
It performs two key functions:
-
Pumps blood through the body, like your heart.
-
Adds oxygen and removes carbon dioxide, like your lungs.
It’s made up of tubes, filters, reservoirs, and oxygenators. Blood leaves your body through a large vein. The machine oxygenates it, warms it, and returns it through an artery.
This process is called cardiopulmonary bypass.
Why it matters:
Without the heart-lung machine, surgeries like valve repair, bypass, and transplants wouldn’t be possible. It literally buys time.
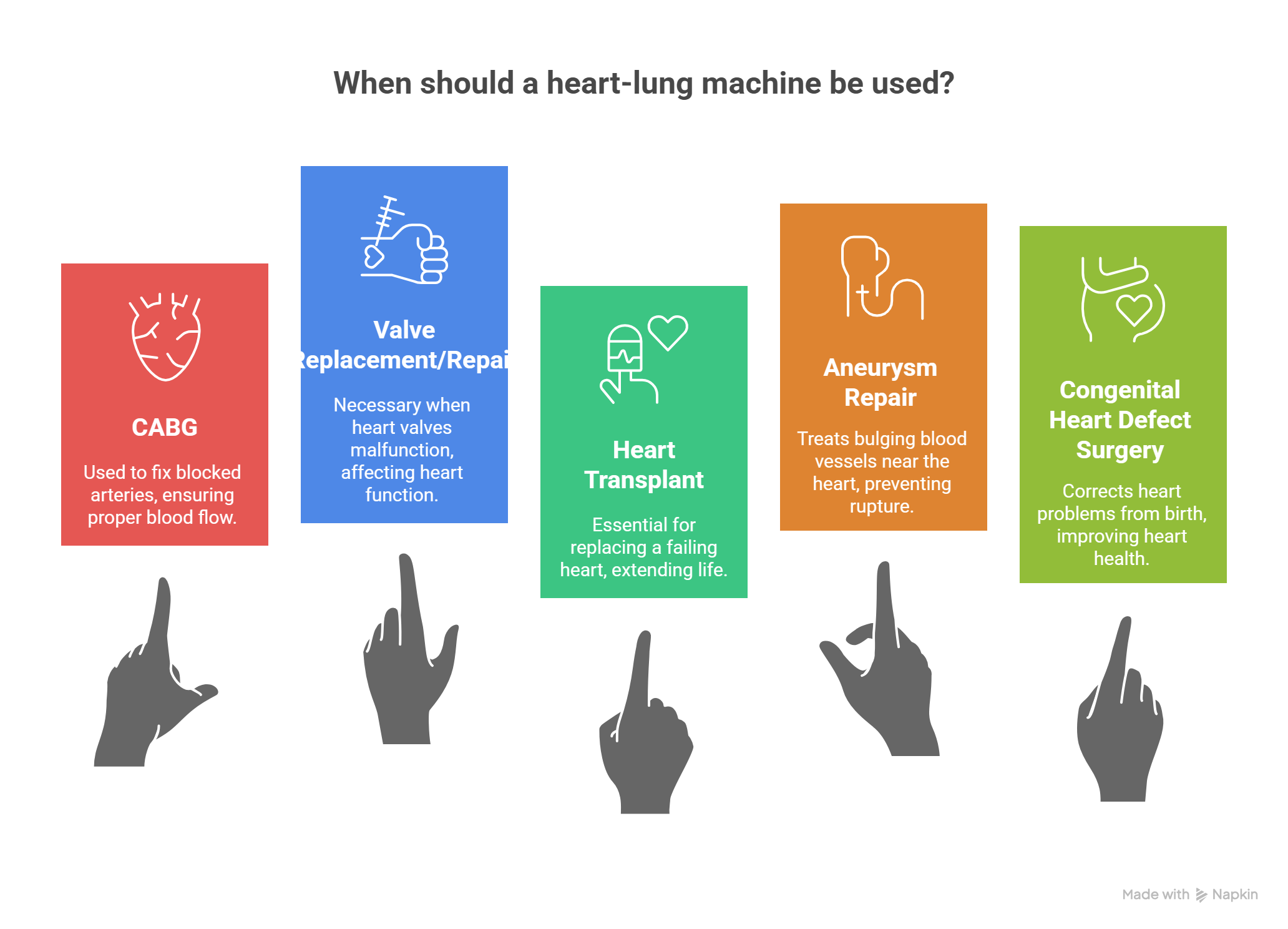
When and Why Is a Heart-Lung Machine Used?
Doctors use a heart-lung machine during major surgeries when they must stop your heart. It keeps blood and oxygen moving while your heart is paused.
Common reasons include
-
Coronary artery bypass grafting (CABG) fixes blocked arteries.
-
Valve replacement or repair—when valves don’t open or close properly.
-
Heart transplants—replaces a failing heart.
-
Aneurysm repair—treats bulging blood vessels near the heart.
-
Congenital heart defect surgeries—corrects heart problems from birth.
These are all life-threatening conditions. The machine gives surgeons time to fix the issue without putting your body at risk.
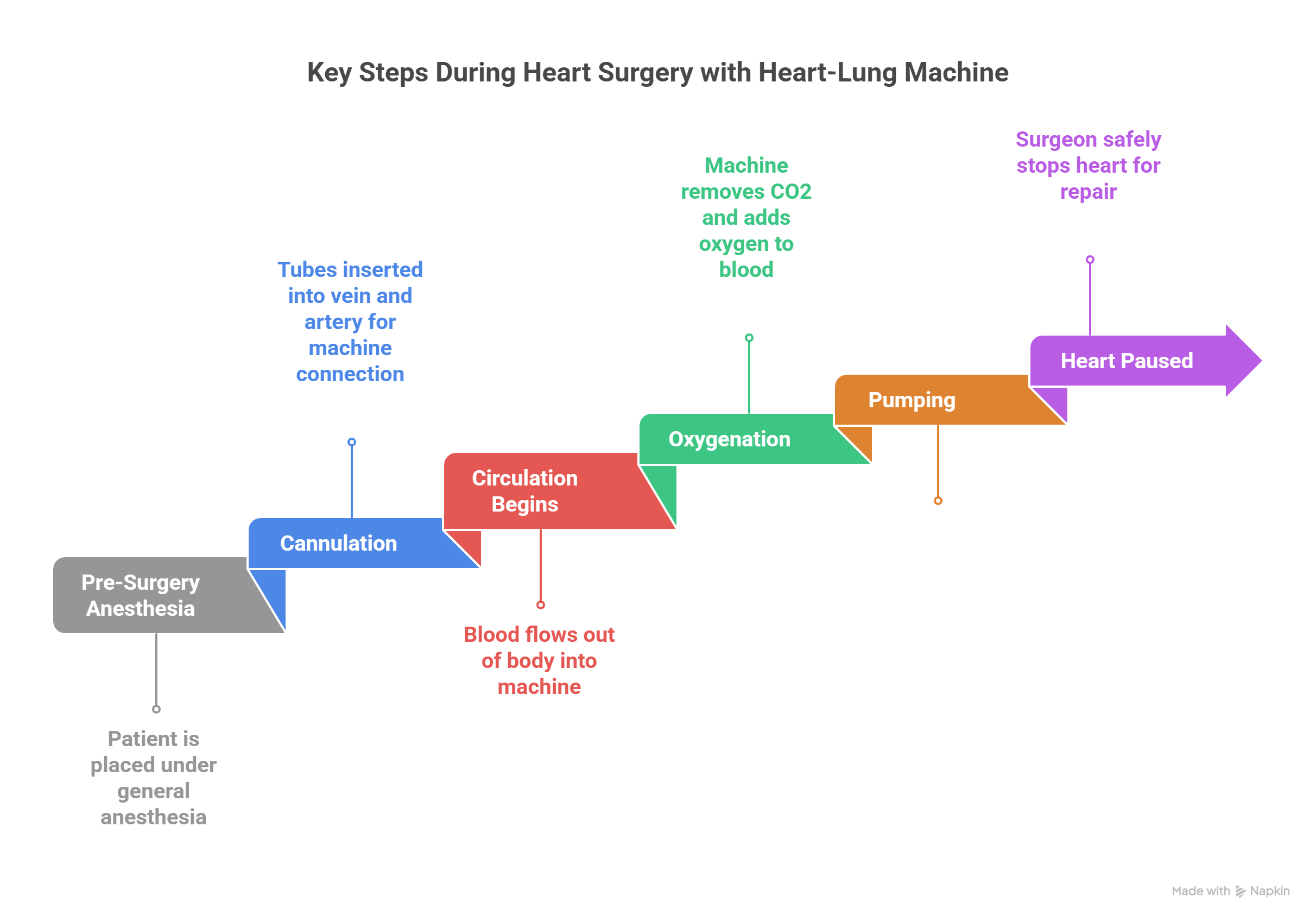
What Happens During the Procedure?
Before surgery, you’re placed under general anesthesia. Once you’re unconscious, doctors make a chest incision and connect the heart-lung machine to your body using large tubes.
Step-by-step process:
-
Cannulation: Tubes are inserted into a large vein and artery, usually near the heart.
-
Circulation begins: Blood flows out of your body into the machine.
-
Oxygenation: The machine removes carbon dioxide and adds oxygen.
-
Pumping: It pushes blood back into your body, keeping vital organs alive.
-
Heart paused: The surgeon stops your heart safely to begin repair.
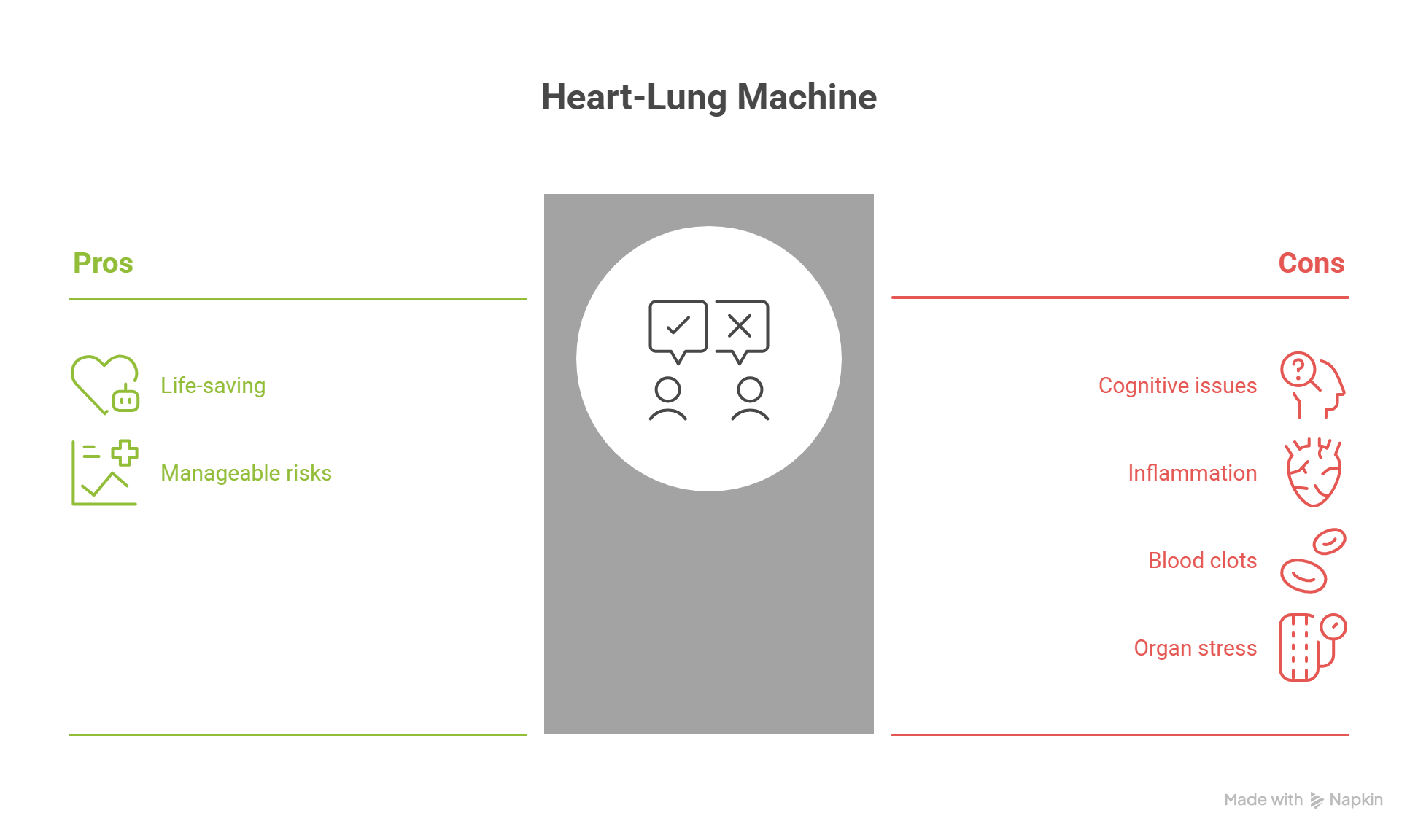
What Are the Risks of Using a Heart-Lung Machine?
While life-saving, the heart-lung machine isn’t without risks. Most patients do well, but it’s important to understand possible complications.
Common risks include:
-
Cognitive issues: Some experience memory problems or confusion after surgery.
-
Inflammation: The machine can trigger an immune response.
-
Blood clots or bleeding: Blood contact with artificial surfaces may increase clotting or bleeding risk.
-
Organ stress: Kidneys or lungs may react poorly in rare cases.
Doctors monitor these risks closely. Most complications are manageable or temporary.
Recovery After Using a Heart Perfusion Machine
Recovery after surgery with a machine varies by person, but there’s a general pattern doctors follow.
What to expect:
-
Intensive care: Right after surgery, patients stay in the ICU for monitoring.
-
Breathing support: Ventilators may help until normal breathing resumes.
-
Gradual movement: Physical therapy often starts within a day or two.
-
Emotional effects: Some feel anxious or depressed, which is normal and treatable.
Recovery takes weeks to months. Nutrition, gentle exercise, and follow-up care speed healing and boost heart health.
The Role of the Perfusionist
Behind the scenes, the perfusionist operates the machine during surgery.
Who they are:
Perfusionists are highly trained specialists in cardiovascular life support. They manage blood flow, oxygen levels, and pressure in real-time.
Why they matter:
-
Adjust machine settings to match your body’s needs
-
Prevent complications like air bubbles or blood clots
-
Support the surgeon and anesthesiologist throughout the operation
Their precision keeps you alive when your heart and lungs can’t. They’re an essential part of every cardiac surgical team.
Risks and Safety Measures Using Cardiac Perfusion Technology
Heart-lung technology are life-saving, but not without risks. Understanding them helps manage expectations.
Possible risks include:
-
Blood clots or air embolism
-
Inflammation or organ stress
-
Temporary memory or cognitive issues (called “pump head”)
-
Bleeding or infection at insertion sites
How risks are reduced:
-
Highly trained perfusionists monitor flow constantly
-
Heparin and filters prevent clotting
-
Sterile environments lower infection risk
-
Machines are routinely inspected and upgraded
These precautions keep surgery outcomes safer and more reliable.
Recovery After Bypass Support
Recovery after cardiac perfusion machine use varies by person and procedure. Most patients begin in intensive care for close monitoring.
Here’s what to expect:
-
First 24–48 hours: Sedation wears off. Breathing tube is removed. Nurses watch vitals constantly.
-
Hospital stay: Usually 5–10 days. Doctors track heart rhythm, oxygen, and healing progress.
-
Physical therapy starts early: Light movement boosts circulation and lung strength.
-
Mental changes: Some patients feel foggy or moody—this fades with rest, nutrition, and time.
Recovery can feel slow. But each step forward rebuilds strength and confidence.
Emotional Support and Family Role
Emotional healing is just as important as physical recovery. Major surgeries involving a heart saving machine can cause stress, fear, and even post-traumatic stress symptoms.
Patients may experience:
-
Anxiety or depression after surgery
-
Fear of recurrence or complications
-
Emotional ups and downs due to medication and trauma
Family support is critical. Loved ones offer stability, motivation, and comfort during this difficult phase. Counseling or cardiac rehab groups help both patients and caregivers process feelings, rebuild routines, and stay encouraged.
Long-Term Outlook and Life After Surgery
Many patients regain full health after heart-lung machine assisted surgery. However, ongoing care is essential.
Key points for long-term success:
-
Follow prescribed medication and lifestyle changes
-
Attend regular check-ups with cardiologists
-
Maintain a heart-healthy diet rich in nutrients
-
Engage in approved physical activity to boost endurance
-
Manage stress through mindfulness or therapy
Adopting these habits reduces risks of further heart issues. It empowers you to live a longer, healthier life.
 9 Tips For Cardiovascular Wellness [2025]
9 Tips For Cardiovascular Wellness [2025]  4 Stages Of Congestive Heart Failure Life Expectancy [2025]
4 Stages Of Congestive Heart Failure Life Expectancy [2025]  Cardiac Output The Heart Metric That Can Save Your Life [2025]
Cardiac Output The Heart Metric That Can Save Your Life [2025]  World Health Day Themes: History, Significance & Global Impact
World Health Day Themes: History, Significance & Global Impact  Did You Know About Constrictive Pericarditis? [2025]
Did You Know About Constrictive Pericarditis? [2025]  How To Improve Heart Rate Variability? [2025]
How To Improve Heart Rate Variability? [2025]  Sperm Count Ways to Improve Male Fertility [2025]
Sperm Count Ways to Improve Male Fertility [2025] 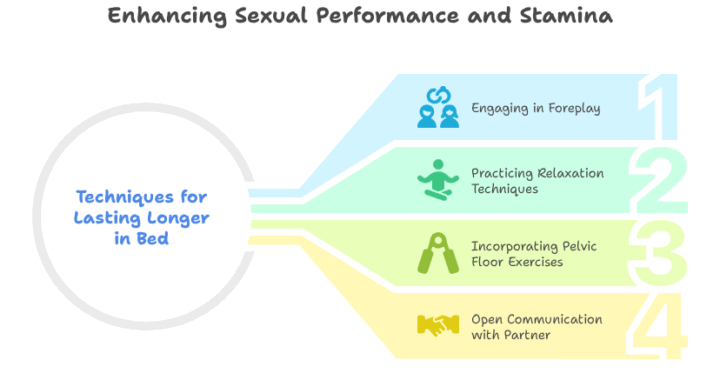 How To Last Longer in Bed Home Remedys That Work [2025]
How To Last Longer in Bed Home Remedys That Work [2025]  Beef Organ Supplements in 2025 [Full Guide]
Beef Organ Supplements in 2025 [Full Guide]  5 Best Fat Burner Supplements [2025]
5 Best Fat Burner Supplements [2025]
Very good
Awesome
Good
Very good
Very good
Very good
Good
Good
Awesome
Good